Background
Effective risk stratification is vital for selecting donors and developing treatment strategies for allogeneic hematopoietic stem cell transplantation (allo-HSCT). Several pretransplant risk models have been proposed to predict post-transplant patient outcomes from pretransplant risk factors. However, it is still challenging to predict mid-to-long-term prognosis. To establish a novel and user-friendly tool for predicting chronic graft-versus-host disease (cGVHD), non-relapse mortality (NRM) and overall survival (OS), we used a Stacked Ensemble Model (SEM) designed to handle right-censored data and competing risk events (Iwasaki et al., 2021).
Methods
Using Japanese registry data, the Japanese Transplant Registry Unified Management Program, we analyzed 21,840 patients who underwent their first allo-HSCT between 2010 and 2018 for hematologic malignancies. Of these, 14,430 patients were alive without cGVHD and relapse on day 100 post-transplantation. Primary endpoint was cGVHD and secondary endpoints were NRM and OS. Data were randomly split into the training set (70% of the dataset) and the validation set (30%). We treated patient age and time from diagnosis to transplant as continuous variables and performance status, ABO type matching, sex matching, disease/status groups based on refined Disease Risk Index, Hematopoietic Cell Transplantation-specific Comorbidity Index, usage of total body irradiation, conditioning intensity, T cell depletion in vivo, human leukocyte antigen (HLA) locus matching, the number of HLA mismatching and CMV serostatus as categorical variables. To evaluate predictive accuracy at day 30, 60 and 100 posttransplant, we considered acute graft-versus-host disease (aGVHD) and its treatment, including grade 2 to 4 aGVHD occurrence, grade 3 to 4 aGVHD occurrence, stage of aGVHD before and after treatment, corticosteroid treatment, anti-thymocyte globulin treatment and treatment response of 1 st line therapy for aGVHD.
Results
The median age of the patients at transplantation was 51 years (inter quartile range (IQR): 39 - 60). The sources of stem cells were HLA-matched related bone marrow (BM) in 967 patients, HLA-matched related peripheral blood (PB) in 1,998 patients, haploidentical BM in 172 patients, haploidentical PB in 778 patients, unrelated BM in 5,539 patients, unrelated PB in 366 patients, and cord blood in 4,237 patients. Myeloablative conditioning was administered in 9,390 patients and reduced-intensity conditioning in 5,040 patients. The most common indication of HSCT was intermediate-risk acute myeloid leukemia (AML) in complete remission (CR, n=3,233) followed by acute lymphoblastic leukemia in first CR (n=2,164) and intermediate-risk AML in non-CR (n=1,618). Median follow-up period of survivors was 2.2 years (IQR: 0.9-4.5).
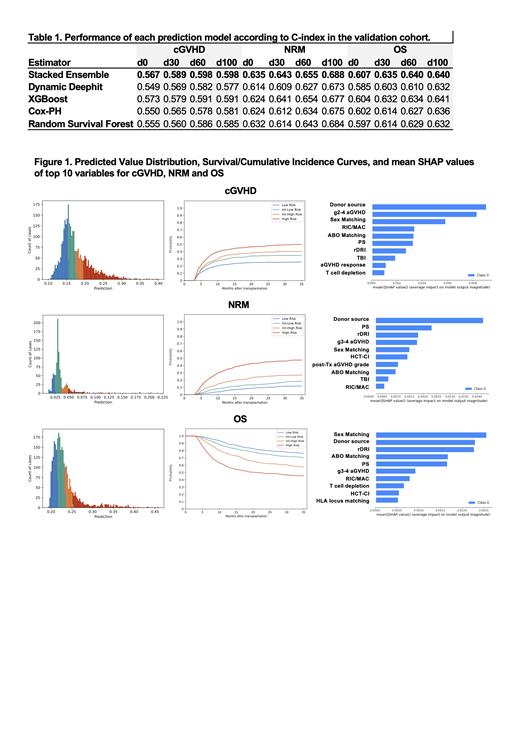
The overall performance of SEM was superior across the endpoints evaluated, cGVHD, NRM and OS, while XGBoost showed a slightly higher C-index for cGVHD, demonstrating its robustness and reliability (Table 1, the C-index for cGVHD/NRM/OS-SEM: 0.567/0.635/0.607, Cox-PH: 0.550/0.624/0.602, Random Survival Forest: 0.555/0.632/0.597, XGBoost: 0.573/0.624/0.604, and Dynamic Deephit: 0.549/0.614/0.589). C-index of SEM for cGVHD, NRM, and OS were gradually improved as time goes by (Table 1, the C-index for cGVHD/NRM/OS: at day 30-0.589/0.643/0.635, at day 60-0.598/0.655/0.640, at day 100-0.598/0.688/0.640).
Kaplan-Meier curves 100-day post-transplantation confirmed the accuracy of our predictions, effectively stratifying patients into four risk groups (Figure 1). SHapley Additive Explanations showed contribution of variables for predicting specific outcomes. Grade 3 to 4 aGVHD and stage of aGVHD after treatment influenced non-relapse mortality. Particularly, grade 3 to 4 aGVHD showed significant impact on OS in line with pretransplant risk factors including sex matching, donor source and disease/status groups. Grade 2 to 4 aGVHD and treatment response of 1 st line therapy for aGVHD influenced cGVHD.
Conclusion
Our study emphasizes the importance of aGVHD events in mid-to-long-term post-transplantation outcomes and presents SEM-based prediction models that account for early-phase post-transplantation events. We are currently developing a user-friendly web application tool for cGVHD, aiming to enhance post-transplant risk stratification and preemptive therapy for cGVHD.
Disclosures
Kanda:Amgen: Ended employment in the past 24 months, Honoraria; Janssen Pharmaceutical K.K.: Honoraria; Novartis Pharma K.K.: Honoraria; Sanofi K.K.: Honoraria; AbbVie Pharma: Honoraria; Megakaryon Co.: Honoraria; Eisai Co.: Research Funding. Atsuta:Otsuka Pharmaceutical Co., Ltd: Speakers Bureau; Meiji Seika Pharma Co, Ltd.: Honoraria; JCR Pharmaceuticals Co., Ltd.: Consultancy; Novartis Pharma KK: Speakers Bureau; CHUGAI PHARMACEUTICAL CO., LTD.: Speakers Bureau. Doki:Janssen Pharmaceutical K.K.: Honoraria; Novartis Pharma K.K.: Honoraria. Tanaka:Otsuka Pharmaceutical: Speakers Bureau; MSD: Speakers Bureau; Kyowa-Kirin: Speakers Bureau; Daiichi Sankyo: Speakers Bureau; Chugai Pharmaceutical: Speakers Bureau; Astellas Phrama: Speakers Bureau; Asahi Kasei Pharma: Speakers Bureau; Abbvie: Speakers Bureau; Pfizer: Speakers Bureau; Sumitomo Pharma: Speakers Bureau. Kanda:AbbVie: Research Funding, Speakers Bureau; Towa Pharma: Speakers Bureau; CSL Behring: Speakers Bureau; Japan Blood Products Organization: Research Funding, Speakers Bureau; Otsuka Pharmaceutical: Research Funding, Speakers Bureau; AstraZeneca: Speakers Bureau; Human Life CORD: Speakers Bureau; Sumitomo Pharma: Research Funding, Speakers Bureau; Amgen: Speakers Bureau; Takeda Pharmaceutical: Research Funding, Speakers Bureau; Meiji Seika Pharma: Speakers Bureau; Asahi Kasei Pharma: Research Funding, Speakers Bureau; Daiichi Sankyo: Research Funding, Speakers Bureau; Saitama Hokeni Kyokai: Speakers Bureau; MSD: Speakers Bureau; Kyowa Kirin: Research Funding, Speakers Bureau; Janssen Pharmaceutical: Speakers Bureau; Sanofi: Speakers Bureau; Pfizer: Speakers Bureau; Chugai Pharmaceutical: Research Funding, Speakers Bureau; Novartis: Speakers Bureau; Bristol Myers Squibb: Speakers Bureau; Precision: Speakers Bureau; Shionogi Pharma: Research Funding; Alexion Pharma: Speakers Bureau; Eisai: Research Funding, Speakers Bureau; FUJIFILM Wako Pure Chemical: Speakers Bureau; Nippon Shinyaku: Speakers Bureau; Wakunaga Pharmaceutical: Speakers Bureau; Taiho Pharmaceutical: Research Funding; Nippon Kayaku: Research Funding; JCR Pharmaceuticals: Research Funding. Sawa:Janssen: Honoraria; Sanofi: Honoraria. Ichinohe:Abbvie Co.: Honoraria, Research Funding; Nippon Shinyaku Co.: Honoraria, Research Funding; Wakunaga Pharmaceutical Co., Ltd.: Research Funding; Chugai: Honoraria, Research Funding; Sumitomo Pharma Co: Honoraria, Research Funding; Takeda Pharmaceutical Co.: Honoraria; Kyowa Kirin: Research Funding; Nippon Kayaku Co.: Honoraria; AsahiKasei Pharma Co.: Honoraria, Research Funding; Novartis: Honoraria; Ono Pharmaceutical Co.: Honoraria; Repertoite Genesis Inc.: Research Funding. Takaori-Kondo:Bristol Myers Squibb: Honoraria; Janssen Pharmaceutical K.K: Honoraria; Otsuka Pharmaceutical: Honoraria, Other: Subsidies ; Megakaryon: Honoraria; Ono Pharmaceutical: Research Funding; COGNANO: Research Funding; DKS Co. Ltd.: Research Funding; Pharma Essentia Japan: Research Funding; Takeda Pharmaceutical: Other: Subsidies; Nippon Shinyaku Co., Ltd.: Honoraria, Other: Subsidies; Kyowa Kirin: Other: Subsidies ; Chugai Pharmaceutical: Other; Eisai: Other; Ohara Pharmaceutical: Other; Kinshikouraininjin: Other; AbbVie: Other; Shionogi Pharma: Other; ASAHI KASEI PHARMA: Other.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal